Hip Resurfacing Surgeon
Many high level athletes, men under 55, and other active individuals do not need a complete hip replacement to alleviate hip pain. For some, hip resurfacing is an excellent alternative. If you have hip pain, you need to be seen by a Hip Resurfacing expert. Dr. Prem N. Ramkumar has the experience and expertise in performing Birmingham hip resurfacing. He is located in Long Beach and serves patients in Los Angeles, Orange County, and surrounding Southern California areas. Contact Dr. Ramkumar’s office today.

What is the hip joint?
The hip joint connects the upper part of the leg to the lower torso. It is surrounded by 20 muscles that attach to the knee, pelvis, and spine. As a result, any major issue originating from the hip joint can cause back pain, knee pain, and pain in the other hip. It is important to note an underlying spine issue can mimic hip findings or coexist with hip findings. The femur (thigh bone) and the pelvis (hip bone) are the two bones that make up the joint. Often referred to as the ball and socket, the ball-shaped surface of the femoral head fits into a cup-like depression of the pelvic bone. Smooth cartilage connects the bones, stabilizing the joint and making it easy to move.
Osteoarthritis of the hip can occur for multiple reasons. Genetics, athletic competition, medical disease (sickle cell, osteonecrosis), medication side effects (corticosteroid use), or unknown reasons can lead to osteoarthritis of the hip. This is a degenerative condition that causes irreversible damage to the hip joint, causing pain and reduced movement. Surgery for arthritis is elective, meaning this is a personal decision when you have decided your quality of life or ability to perform activities of daily living are suffering. The definitive surgical treatment for end-stage hip arthritis – both osteoarthritis and inflammatory arthritis – is total hip replacement, also known as total hip arthroplasty.
How does hip resurfacing differ from a total hip replacement (THR)?
Both hip resurfacing and traditional total hip replacements are designed to improve your activity, restore your physical function, and decrease your pain. The socket is replaced in both operations with a metal shell. In a traditional total hip replacement the head and neck are removed and the femur is rodded with a stem. In a hip resurfacing, however, significantly more bone is preserved as just the diseased portions of the head are removed and sculpted to accept a metal cap. The preservation of the neck offers preservation of more natural movements, range of motion, and higher impact loading activities. Not entering the femur with a rod means no changes to leg lengths and slightly less medical risk during surgery.
Patients who are younger and would like to continue higher demand activities that require more impact or more range of motion are better suited for hip resurfacing, if they are appropriate candidates. Several professional athletes have successfully returned to a high level of athletics following their hip resurfacing with the BHR: Andy Murray, Isaiah Thomas, Tiago Splitter, Ed Jovanovski, Colby Lewis, Artur Akhmatkhuzin, John Starks.
Patients who are older or lower demand and want to return to basic activities of daily living are better candidates for traditional total hip replacement.
Why do more people not offer hip resurfacing?
Hip resurfacing arthroplasty is not offered by most surgeons for several reasons:
- Education and exposure
- Only a handful of teaching orthopedic surgeons at academic institutions perform the procedure. The key thought leaders performing the operation at a high volume are based out of Washington University in St. Louis, Hospital for Special Surgery, and the Cleveland Clinic. Dr. Ramkumar was fortunate enough to train at two of those three institutions. Because the education and exposure to this specialized operation is concentrated to a few areas, very few are exposed to a balanced understanding of the procedure – from its strengths to its limitations.
- Technical difficulty
- Performing the operation requires a deep understanding of the implant design and biomechanical properties, which differ greatly from that of traditional total hip replacements. Although both hip resurfacing and total hip replacements replace the socket, they are inserted in very different positions. Similarly, the femoral head size requires extra caution and consideration that add more surgical time and effort when compared to a traditional total hip replacement.
- Additional certification
- To perform the operation, additional credentialing and training is required by the manufacturer to be an eligible surgeon to implant the Smith & Nephew Birmingham Hip Resurfacing (BHR) implant. This is the only FDA approved implant on the market with a successful track record spanning over two decades.
- Confusing Narratives
- The BHR is a metal-on-metal (MoM) implant. MoM has been associated with poor outcomes and well-deserved negative media attention when they were used for traditional total hip replacements. The failures for these MoM traditional total hip replacements occurred at the junction of the artificial stem and the artificial head, known as the trunnion. Hip resurfacing implants do not have a trunnion, as only the femoral head is touched in the operation. Thus, applying the poor outcomes of MoM total hip replacements to hip resurfacing simply does not apply. MoM bearings have been used since the 1950s with good long-term results and no concern for failure at the head-socket junction, which is the only junction that exists in hip resurfacing.
- In 2010, there was a very public worldwide recall of the DePuy (Warsaw, Indiana, USA) ASR Hip Resurfacing and Total Hip Replacement systems. The recall was for unsafe metal ion levels that destroyed surrounding structures and caused early failure. For their total hip system, metal-related complication occurred at the trunnion, which does not exist in hip resurfacing as previously mentioned. This recall helped us appreciate the importance of eliminating the use of MoM in traditional total hip replacements worldwide. For the ASR hip resurfacing system (and other hip resurfacing systems that failed in a less public fashion), failures were later found to be due to deviations in the manufacturing and design process (poor metallurgy, socket design, clearance, and sphericity). In some instances, the manufacturers altered implant production to reduce costs, which compromised the product and made it more prone to failure. As a result, this gave all hip resurfacing implants a bad reputation.
- The BHR hip resurfacing implant specifically, unlike the previous failed resurfacing implants, has an ideal design (metallurgy, socket design, clearance, and sphericity). It also has a meticulous manufacturing process. To this day, the BHR requires a great deal of resources to manufacture and remains one of the few implants on the market that still depends upon manual labor to produce each and every implant. Additionally, the BHR requires special training and certification before a surgeon is permitted to use the implant given its many nuances. When you combine all these unique barriers and considerations compared to traditional total hip replacement, it is clear why performing hip resurfacing with the BHR can be a tedious process. However, survivorship track record of the BHR implant is on par or better than traditional total hip replacements – which is remarkable considering the patient population is younger and higher demand. The BHR is the only hip resurfacing implant Dr. Ramkumar uses as it is time tested and deservedly the only FDA-approved hip resurfacing implant.
Who is a candidate for Birmingham hip resurfacing (BHR)?
Hip resurfacing is not suitable for everyone. Dr. Ramkumar only performs the procedure on patients who meet specific criteria:
- Highly active individuals such athletes or skilled laborers
- Males
- Under the age of 65
- Have amenable bone architecture: bone quality, femoral head size, no extreme version abnormalities
- No chronic kidney disease, dialysis, or prior kidney transplants
- Ability to follow-up: you will need annual checks with imaging and bloodwork for the first 5 years then again at 10 years
BHR historically has not worked well on women because they tend to have smaller and more variable bony architecture, specifically femoral heads. Additionally, younger women of childbearing age risk the potential of metal ions passing across the placenta to a fetus that is not able to yet clear these ions at the rate of an adult with normally functioning kidneys. As a result, women are not candidates for this operation.
How is Birmingham hip resurfacing performed?
Before the surgery begins, the patient receives a spinal anesthetic and sedation medication. Once the patient is asleep, Dr. Ramkumar makes an incision over the affected hip and carefully exposes the joint. Special instruments will be used to trim and reshape the femoral head to cement it in with a metal cap. The patient can either go home or spend one night in the hospital. The patient is allowed to walk the same day with 75% weight bearing allowed and no active abduction to give the body time to heal. An anti-inflammatory medication will be given to prevent the development of heterotopic or aberrant bone formation unique to the procedure.
Dr. Ramkumar will give you specific post-surgery instructions to reduce pain and swelling. Recovery time varies from person to person, but you should be able to walk within a few weeks and return to normal activities within six weeks.
Hip Resurfacing Q&A
1. What are the risks of hip resurfacing with the BHR?
General Risks: The general risks of hip resurfacing are the same as with traditional total hip replacement. These include infection, dislocation, blood clots, nerve injury, and extra bone formation around the hip that could make the hip stiff. The risk of infection with hip resurfacing is no different than with total hip replacement. The risk of dislocation is 10x lower, because of the larger diameter ball. The risk of extra bone formation around the hip are slightly higher with a hip resurfacing because of the need to work around your bone in an enclosed space, although this is commonly prevented with an oral medication.
Femoral Neck Fracture: A risk unique to hip resurfacing that is not present in traditional hip replacement is that of femoral neck fracture. The femoral neck is a vulnerable area of bone that connects the ball of your hip joint to the rest of your thighbone. When elderly people fall and “break their hip”, this is the area that breaks. With a traditional hip replacement is done, this bone is removed, so it cannot break. With a hip resurfacing, the femoral neck is preserved, so there is a risk of fracture. We believe the risk of fracture in this area is between 1-2%. It is because the surgical exposure, preparation of bone, and placement of the component with cement may cause this bone to be more vulnerable. Following postoperative instructions and not doing too much too early will be critical to avoid this risk.
The risk of femoral neck fracture is why crutches are necessary for 3-4 weeks post-operative and impact activities are not recommended for 6 months. If you have a femoral neck fracture after hip resurfacing, you will need another operation to convert it to a traditional total hip replacement.
Routine Follow-Up Required: Another unique element Dr. Ramkumar insists upon for patients who undergo hip resurfacing is the need for routine follow-up. This operation inherently requires more surveillance, including x-rays, MRIs, and bloodwork to ensure there are no looming concerns. Although rare, metallosis is a possible risk that could damage surrounding musculature if left untreated. If you have any new pain or dysfunction after recovery from the operation, you must return as soon as possible for evaluation. Otherwise, annual surveillance remains critical – especially in the first five years.
2. What will happen when the hip resurfacing wears out?
When a hip resurfacing wears out, it is generally because the femoral cap loosens from the underlying bone. If this happens, it can be converted to a traditional total hip replacement with a stem in the thigh bone, utilizing a big metal ball to match your socket. Generally, the socket is firmly attached to your bone and will not need to be revised.
3. What are the major benefits of hip resurfacing?
The major benefit to resurfacing compared to traditional replacement is the preservation of bone. For patients who may outlive their implant, this is a tremendous advantage. Since bone is preserved at the initial operation, more bone is available for the next operation.
A hip resurfacing also has a larger diameter ball, which gives a greater theoretical range of motion. It is also more stable, so the dislocation rate is lower. Additionally, a hip resurfacing loads the bone of the femur the way it is in your own hip, so we believe you can return to more impact activity.
4. Should I be concerned about the metal ions that are released into the blood?
This is a controversial topic. There have been many studies looking at this issue, and none have been conclusive. People with healthy kidneys excrete the metal ions in the urine. At baseline we have metal ions in our body and they exist in the water we consume. Metal/metal hip replacements have been around since the 1970’s, and they have never been linked to an increase in cancer or other diseases. We do not know “safe levels” of these metal ions in the blood, nor is it likely that we will be able to determine “safe levels” in the near future. Because metal ions are excreted by the kidneys, we do not perform MoM hip resurfacing in patients on dialysis, have had a kidney transplants, or are in renal failure.
5. What kind of activity can I do after resurfacing?
Once the healing process has completed and the bone around the implants has strengthened, there are no restrictions whatsoever. This takes up to a year for the bone to fully mature. Patients are able to return to martial arts, shipyard work, police duty, dancing, yoga, swimming, cycling, basketball, ice hockey, firefighting, weight lifting, and competing in triathlons and marathons.
Dr. Ramkumar discusses all the potential benefits and risks with each patient before surgery.
6. What can I expect before and after the total Birmingham Hip Resurfacing surgery?
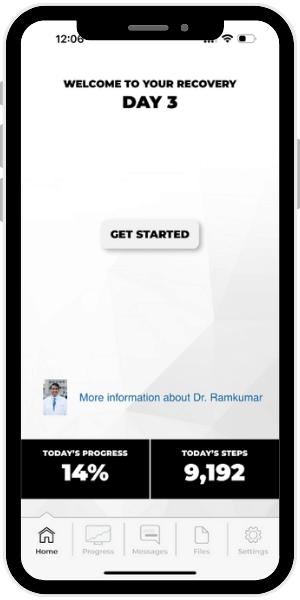
Dr. Ramkumar emphasizes the importance of establishing clear expectations and providing comprehensive pre- and post-surgery education. This proactive approach not only alleviates anxiety but also leads to an enhanced overall surgical outcome.
What does the process look like leading up to BHR surgery?
We follow a detailed process and checklist to ensure your safety prior to undergoing hip resurfacing. Although hip resurfacing is becoming a more common operation, it is a very important life event, and we want to minimize as many preventable risks as possible.
Learn more >> Preoperative Assessment for Joint Replacement/Resurfacing Surgery
What happens after BHR surgery?
Our post operative guidelines offer an overview of what you can expect after your surgery, such as:
- How do you address pain management and nausea after surgery?
- Between all the medications and physical therapy, what do the first few days look like after surgery?
- What do the first few days look like after surgery?
- What activities can I do right after surgery?
- Is swelling and bruising after surgery normal?
- Is it normal to have sleep issues after hip replacement and what can I do about it?
- When can I bathe after surgery?
- When can I drive after surgery?
Learn more >> Postoperative Guidelines for Joint Replacement/Resurfacing Surgery
7. Which professional athletes have successfully returned to a high level of athletics following their hip resurfacing with the BHR?
Andy Murray, Isaiah Thomas, Tiago Splitter, Ed Jovanovski, Colby Lewis, Artur Akhmatkhuzin, John Starks have all openly discussed the success of their BHR hip resurfacing surgeries which have been performed by Dr. Ramkumar’s peers.
Selecting an orthopedic hip surgeon with experience performing Birmingham Hip Resurfacing is crucial to a positive outcome. Dr. Prem Ramkumar is located in Long Beach and serves patients in Los Angeles, Orange County, and surrounding Southern California areas.
Would you like more information about hip resurfacing?
Below are several studies that have been done about hip resurfacing. Dr. Ramkumar is also happy to do an email consultation.
2 – Results of Birmingham hip resurfacing at 12 to 15 years: A single-surgeon series.
4 – Socket position determines hip resurfacing 10-year survivorship.